Moderate Scoliosis
There is a High Potential of Progression
As a progressive and incurable condition, scoliosis, if left untreated, is virtually guaranteed to get worse over time. This is why it’s important to understand its progressive nature so we can try and stay ahead of its progressive line. The majority of my patients are in the moderate stage because this is when the condition tends to produce noticeable changes that lead to a diagnosis and treatment.
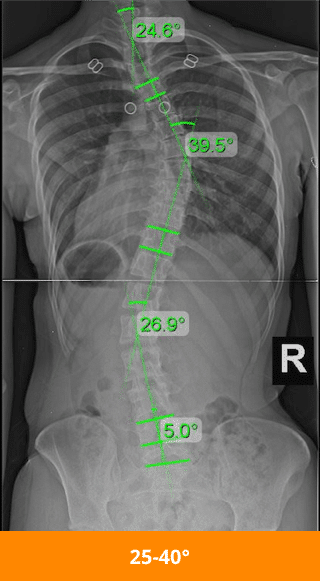
When a scoliosis diagnosis is given, the patient is told whether it’s mild, moderate, or severe. This classification is based on a measurement taken via X-ray known as ‘Cobb angle’. A patient’s Cobb angle tells us how far out of alignment the spine bends and twists. Cobb angle measurements between 25 and 40 degrees, with rotation, are classed as ‘moderate scoliosis’.
Before we move on to the specifics of moderate scoliosis, and how adult and adolescent scoliosis can differ, let’s first talk about how the condition is defined, classified, and why this is the stage in which most adolescents are diagnosed.
What Is Moderate Scoliosis and How is it Classified?
Scoliosis is defined as an abnormal spinal curvature that bends to the side and includes rotation. It’s the rotation that tells us the scoliosis is structural and not a postural issue.
Once a condition moves into the moderate stage, it has moved into a gray area. The condition has progressed beyond the mild stage and has likely started to produce noticeable symptoms, but it is still not considered severe.
Depending on the chosen treatment approach, moderate conditions are either observed or actively responded to, which we will return to later.
As mild scoliosis often only produces subtle signs that would go unnoticed by the average person, this is why the majority of my patients are in the moderate stage: because it’s during this stage that the condition most often becomes noticeable.
At the point of moderate scoliosis, the condition has already progressed, as virtually all conditions are guaranteed to do, and while the speed of that progression is impossible to predict, fast or slow, it will happen.
Before we move on to specifics of moderate scoliosis, let’s first talk about how the condition is classified.
Condition classification is based on important characteristics of the patient and their condition such as Cobb angle, age of patient, cause (if known), and location of the curvature.
Cobb Angle
If a patient’s spine bends to the side, rotates, and has a Cobb angle measurement of between 25 and 40 degrees, this is considered ‘moderate scoliosis’.
Cobb angle is considered the gold standard for assessing scoliosis as it tells us where the condition fits on its severity scale.
Cobb angle is measured via X-ray and involves drawing intersecting lines from the most tilted vertebrae of the curvature.
A patient’s Cobb angle tells us if their condition is mild, moderate, or severe, and once we know the condition’s severity level, we can move forward with designing a treatment plan that accounts for likely symptoms and potential related complications.
Patient’s Age
Patient age is crucial in classification as it indicates health, fitness levels, and likely symptoms.
For instance, in adolescent idiopathic scoliosis (AIS), pain is usually minimal because adolescents’ spines are still lengthening, counteracting compression of the spine, muscles, and nerves. However, adults with moderate scoliosis often experience more pain.
Age also helps predict progression. While the exact cause of AIS is unknown, growth is the primary trigger for progression.
Adolescents are at high risk for rapid progression, whereas adults are not, so treatment plans differ accordingly.
Condition Cause
If a patient with moderate scoliosis is between 10 and 18 years old with no known cause, it’s classified as adolescent idiopathic scoliosis (AIS).
‘Idiopathic’ means the condition has no single known cause and is considered multifactorial, varying from person to person. AIS accounts for 80% of diagnosed cases, while the remaining 20% are due to less common forms like neuromuscular, congenital, degenerative, or traumatic scoliosis.
Understanding the cause is crucial because in atypical forms, scoliosis develops as a secondary complication of a larger medical issue, guiding the treatment approach. Identifying if the condition is idiopathic or has a known cause helps us determine the appropriate treatment.
Location of the Curvature
The spine has three main sections: cervical (upper back and neck), thoracic (middle back), and lumbar (lower back).
Curvatures most commonly develop in the thoracic spine. Knowing the curvature’s location guides treatment and indicates symptoms and complications.
A diagnosis of moderate adolescent idiopathic thoraco-lumbar scoliosis tells us the severity (moderate), patient age (adolescent), cause (idiopathic), and location (thoracic and lumbar).
Now that we have explored moderate scoliosis in terms of definition, diagnosis, and classification, let’s discuss the benefits of early detection. If you suspect moderate scoliosis, reach out to us; early treatment has many benefits.

Moderate Scoliosis and Early Detection
As a progressive and incurable condition, it’s highly beneficial to spot the condition early on because this means treatment can also be started early on.
The more mild a condition is at the time of diagnosis, the easier it is to treat, and the more likely the patient is to experience positive treatment results in the form of a curvature reduction.
Most often, individuals with moderate scoliosis are diagnosed in adolescence. This is the case because, as previously mentioned, early detection of mild scoliosis, the stage that comes before, is very challenging.
To me, when a patient’s condition is in the mild or moderate stage, this is precisely the time to start treatment because we want to avoid their progression into the severe stage.
While the rate of scoliosis progression differs from one patient to the next, progression is inevitable, unless a proactive approach is taken.
As moderate scoliosis tends to be when individuals and their families actually notice scoliosis-related symptoms such as postural changes, diagnosing moderate scoliosis is less of a challenge than with milder forms.
This leads us to the next topic of interest: symptoms of moderate scoliosis.
Symptoms of Moderate Scoliosis
While every case is different, moderate scoliosis generally produces some telltale signs and symptoms.
It’s important for parents and caregivers of adolescents to know some of these common indicators to look out for so the condition can be diagnosed and treated, before it progresses into the next severe stage of progression.
As scoliosis is a spinal disorder and the brain and spine work in tandem to form the central nervous system, the condition can be felt in multiple areas of the body, other than just the back.
Some scoliosis symptoms seem unrelated, such as headaches, but spinal disorders can cause a ripple effect throughout the body and produce a myriad of symptoms.
Moderate Scoliosis Pain
For adolescents, scoliosis is rarely painful, but as the curvature worsens, pain can increase. About 20% of adolescents report muscle pain due to compensating for the abnormal curvature, especially in the cervical spine.
Adults experience scoliosis pain differently. Their spines are no longer growing, so compression affects the spine, muscles, nerves, and tissues. Pain often brings adults in for treatment.
Moderate scoliosis in adults is usually idiopathic or degenerative. Idiopathic scoliosis means they had it in adolescence but were unaware. Symptoms like pain often emerge in adulthood, including back and neck pain, radiating pain, and hip pain due to pelvic asymmetry.
Degenerative scoliosis results from age-related spinal changes, often involving the intervertebral discs. As these discs degrade, the spine can slip, rotate, and bend abnormally, causing scoliosis and pain.
Postural Changes
As every case of scoliosis is different, even within ‘moderate scoliosis,’ there can be a wide range of symptoms.
Not everyone with moderate scoliosis will have all the following postural changes, but these are the most common signs indicating moderate scoliosis affecting posture and symmetry:
- Clothing not fitting or hanging unevenly
- Arms appearing to hang at different lengths
- One hip appearing higher than the other
- Legs seeming to hang at different lengths
- Ribs sticking out more on one side
- One shoulder blade protruding more on one side
- Shoulders appearing unbalanced
- Head not centered over the torso
- Uneven waistline
These postural changes lead to an overall asymmetrical appearance and can affect the way a person walks.
Sleep and Digestive Issues
As scoliosis progresses, related symptoms and potential complications become more noticeable. Scoliosis can disrupt sleep due to discomfort and pain, making it difficult to get comfortable.
Lung impairment, though more common with severe scoliosis, can also affect sleep quality by making breathing more difficult.
Scoliosis can impact the body in various ways because the spine and brain form the central nervous system (CNS), which facilitates communication throughout the body. Messages passing between the brain and spine affect almost every system in the body, which is why some scoliosis symptoms can seem unrelated.
An abnormal spinal curvature can impact the digestive tract as much as it affects the muscles near the spine, leading to digestive issues and impaired bowel movements.
Headaches
Headaches are not always a part of someone’s scoliosis experience, but they are a common complaint.
Headaches can be a symptom of mild, moderate, and severe scoliosis, and will likely vary in intensity based on condition severity.
Especially associated with curvatures of the cervical spine (upper back and neck), tight neck muscles can place adverse tension on the head and cause tension headaches to occur.
In addition, scoliosis can affect the flow and levels of cerebrospinal fluid that cushion and protect the brain and spinal cord.
When CSF levels in the brain are low, this can also lead to headaches. It’s not uncommon for scoliosis-related headaches to become debilitating and reach migraine status.
Balance and Equilibrium Issues
As you can imagine, when the spine has an abnormal curvature, the body’s overall shift can be felt in multiple ways.
In addition to an overall asymmetrical appearance that can develop and changes to the way a person walks, a person with scoliosis can also struggle with balance and coordination.
Issues with proprioception can emerge: the body’s ability to recognize its position in the absence of visual cues.
If an average person were to close their eyes and stand on one foot, they could likely do this quite easily, but for someone with scoliosis, this can be difficult.
Changes in Gait
I can tell a lot about a patient’s condition by the way they walk.
In cases of moderate scoliosis where postural changes are more extreme and noticeable, what I see a lot of are arms that are held closely to the sides, instead of naturally swinging back and forth during movement.
As the normal counter-rotating movement of the shoulders and hips are compromised, this can noticeably change how a person walks and holds themselves.
Changes to gait are also connected to balance and equilibrium issues.
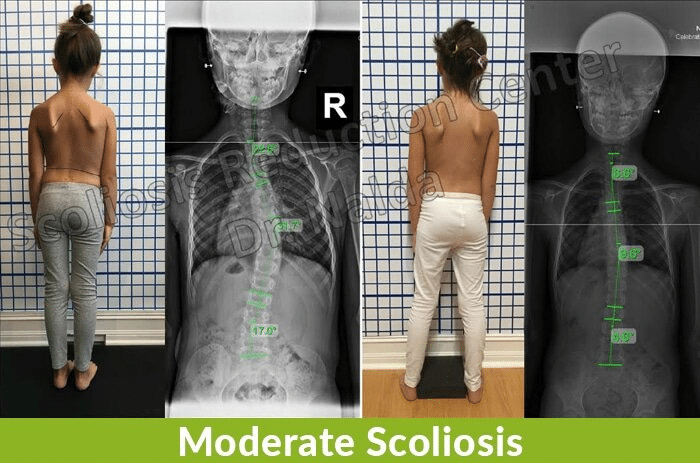
Take a look at the accompanying images of Carrie to get an idea of what moderate scoliosis looks like, not to mention how different the same spine can look after a reduction.
You can also see the difference in shoulder blade symmetry with one protruding more on one side, and in the after-treatment image, you can also see how much that postural symptom has improved with treatment.

Moderate Scoliosis Progression
‘Progression’ is a fancy medical term that refers to a condition or disease getting worse.
When it comes to treating any progressive condition like scoliosis, the goal is to somehow stay ahead of its natural progressive line.
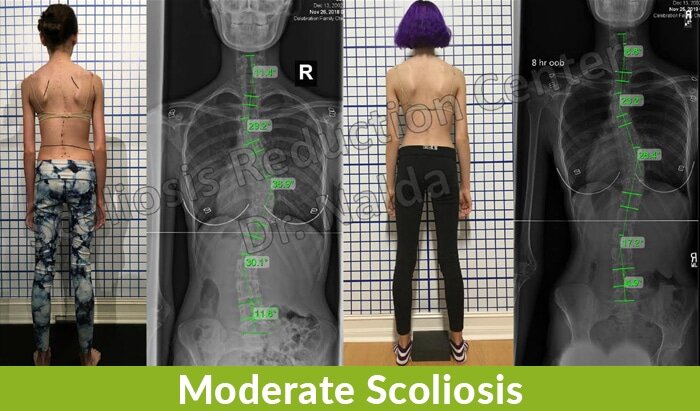
If you take a look at Sheila’s X-ray images before and after treatment, you can see how much of an impact active treatment can make. You can see how much straighter her spine is and how significantly the Cobb angle measurements have decreased.
As looking at the images shows how positively active treatment can impact a conditon’s progression, you can imagine how, conversely, a patient’s condition can be impacted negatively by not engaging in active treatment.
Treatment success for progressive conditions means either stopping the condition’s progression indefinitely, or putting off its progression for as long as possible.
For those who have progressed from mild to moderate, the reality is their condition is virtually guaranteed to get worse and reach its severe stage; this is especially true if active and preventative treatment efforts aren’t made.
As already mentioned, the most common age group diagnosed with scoliosis are adolescents between the ages of 10 and 18.
This age group is entering into a significant stage of growth and development, and as we know that growth is the biggest trigger for progression, we know that these patients are facing a high risk of rapid progression.
When it comes to adults with moderate scoliosis, although the progression might slow down once skeletal maturity has been reached, progression is still a factor. Even at a seemingly glacial pace of one degree a year, over 10 years, there is a cumulative effect that really adds up.
In addition to the majority of adult scoliosis cases that are continuations of AIS, the other common form of adult scoliosis is degenerative.
When paired with the natural degenerative effects of aging on the spine, such as intervertebral disc issues, progressive rates in adulthood can increase. In fact, the larger a curvature gets, the more likely it is to keep getting larger.
This is why early treatment is so important and beneficial: so the condition can be impacted on a structural level and that progressive line can be slowed down or stopped.
Now that we have explored the progressive side of moderate scoliosis, let’s move on to the two main treatment approaches patients have to choose between: traditional and functional.
Moderate Scoliosis Treatment Options
We all face those moments in life that have the power to impact what comes next. For people with scoliosis, one of these big fork-in-the-road moments is choosing how to treat their condition.
This is never an easy decision to make as it can have life-long repercussions, so there is a lot of pressure on patients and their families to make the best possible choice.
The challenge of facing this decision and the importance of it led me to write Scoliosis Hope; in it, I devote a lot of time to explaining how scoliosis-treatment options have evolved over the years.
I do this because I want to empower patients and their families with the knowledge that a diagnosis of moderate scoliosis does not have to mean passivity and surgery; it can mean action and results.
Before we get to the details of our proactive functional approach here at the Center, let’s first take a look at what the traditional treatment approach would typically recommend to patients with moderate scoliosis.
Traditional Treatment Approach for Moderate Scoliosis
For those on the traditional treatment path for their moderate scoliosis, they would be doing a lot of watching and waiting.
Early detection is not as important for those undergoing traditional treatment because in the mild and moderate stage of the condition’s progression, the main response is to observe how/if the condition is progressing, rather than actively treat it.
The issue I have is that, especially once a case has already progressed from mild to moderate, the condition’s progressive line is going to keep moving forward.
So, basically, patients on this path might have been diagnosed while their condition was in its mildest form, but they wouldn’t have engaged in active treatment anyway.
Most often, patients receive their diagnosis while already in the moderate stage; this is because the symptoms produced during the mild stage are so subtle they often go unnoticed.
It’s common that it’s not until a patient reaches the moderate stage of progression that their condition starts to become noticeable and leads to a diagnosis.
The strategy behind the traditional treatment approach is to observe the condition until it gets to a certain point (the surgical threshold), and then recommend spinal-fusion surgery as the best option.
In the traditional approach, the underlying goal is to slow/stop progression; it’s not to actually ‘correct’ the spinal disorder. While this might not seem like a clear or particularly important distinction now, it will make sense once we start exploring our treatment approach here at the Center.
While the traditional approach is more reactive than proactive, one form of treatment that is often introduced during the moderate stage is bracing with the Boston brace.
Bracing and Moderate Scoliosis in Traditional Treatment
Patients who have progressed from mild to moderate scoliosis can be prescribed a squeezing type of brace; the most common type of brace used in the traditional approach is the Boston brace.
The idea behind this is that the brace will stabilize the spine and prevent the abnormal curvature from getting worse.
The Boston brace does this by aligning pads with the most tilted section of the curvature. The pads put pressure on the abnormal curvature and squeeze the spine to limit its movement and progression.
The goal with this is to control progression in the moderate stage so that the patient’s curvature doesn’t reach the severe stage and reach that surgical threshold of 40+ degrees.
Even if the Boston brace is successful at holding a person’s progression in the moderate stage, it will never reverse curvatures, and adolescents can also experience a worsening of their condition, despite complying fully with the brace prescription.
This brings us to a big issue with bracing as a treatment option for adolescents with scoliosis: compliance.
Compliance
With the use of traditional braces such as the Boston, in order for the brace to be truly effective, it has to be worn for approximately 21 hours a day.
Now, considering the most common age group diagnosed with scoliosis, adolescents between the ages of 10 and 18, compliance can be an issue.
It can sometimes be difficult to convince a teenage patient of the merits of bracing, but this can also be said of different types of braces.
In addition, the Boston brace is rigid, bulky, and uncomfortable. Most teenagers just want to fit in; they don’t want to stand out.
The reality is for many teens wearing their brace to school, that brace comes off and stays in the locker until home time. If the rules of the brace are not complied with 100 percent, its potential efficacy is greatly reduced.
Bracing may or may not impact progression in a positive way, but what it very likely will do is impact adolescent wearers emotionally and socially.
This is another benefit to starting active treatment while the condition is in its mildest form, so the patient doesn’t have to face the hardships of bracing in the moderate stage.
So the Boston brace, and other traditional braces like it, have the end goal of stopping/slowing progression. It does this by squeezing the spine into a corrective position and holding it in place in the hopes of stabilizing it; here at the Center, we use a different type of brace (corrective) that helps us work towards achieving a structural curvature reduction.
When we explore a different type of bracing alternative that we use in our functional treatment approach, you’ll see that not all braces are created equal.
For those moderate scoliosis patients walking the traditional treatment path, a question they are likely to ask at some point, especially if bracing has proven ineffective, is whether or not their condition requires surgery.
Before we move on to the different treatment options our functional approach offers moderate scoliosis patients, let’s first explore how the traditional approach funnels patients towards spinal-fusion surgery.
Does Moderate Scoliosis Require Surgery?
The quick and simple answer to the question of whether or not moderate scoliosis requires surgery is ‘no’.
This is because moderate scoliosis curvatures would have a Cobb angle of between 25 and 40 degrees; the degree of curvature considered severe enough for surgery is 40+.
However, for those in the moderate stage of scoliosis progression, there is only one stage that comes after, and that stage (severe scoliosis) is the stage in which many patients have spinal fusion recommended to them.
In most cases, if bracing has proved ineffectual at controlling progression, and the curvature increases to 40+ degrees, this is considered entering into the surgical threshold.
For those with moderate scoliosis, the most important thing to remember is that as long as their condition remains ‘moderate’, their degree of curvature has not reached that surgical threshold; however, if left untreated, or not treated actively, moderate scoliosis is one progressive stage away from entering into the surgical threshold.
This is why I feel moderate scoliosis is the time to act decisively so that the patient doesn’t have to face the agony of making that choice, not to mention the heavy side effects and risk of complications that spinal fusion comes with.
Potential Spinal Fusion Side Effects and Complications
First off, spinal fusion, like the overall treatment goal of the traditional approach, doesn’t have ‘correction’ as its end goal; its goal is to stop progression.
While the surgery can work to stop progression in some cases, there is no guarantee that it will do so, and for those hoping surgery will ‘fix’ their scoliosis, this is simply not the case.
As spinal fusion involves fusing the most-tilted vertebrae of the curvature into one solid bone to eliminate movement in the area, this can also eliminate progression, but what it also does is remove flexibility in that section of the spine.
Many patients are disappointed with their post-surgical flexibility limitations.
In addition, while many patients opt for surgery to reduce scoliosis-related pain, some report an increase in pain after the procedure, and this can be very disheartening.
Spinal-fusion surgery is not only costly monetarily, but also comes with the potential for developing some pretty serious side effects and/or complications: pain, infection, excessive bleeding, fusion failure, hardware failure, adverse reaction to hardware, nerve damage, paralysis, and more.
There is also a huge gap in the existing research on how spinal fusion affects people in the long term, as in 20, 30, and 40+ years down the road.
Spinal fusion is an invasive and lengthy procedure, and its effects are permanent; there is no un-fusing a fused spine, and the only recourse for people whose fusion has failed is more surgery.
This is why I consider spinal fusion as a last resort, as a treatment option for extreme cases where other more natural approaches have first been tried and failed.
This leads us into the approach we offer here at the Scoliosis Reduction Center®: a noninvasive and natural functional treatment option.
Functional Treatment Approach for Moderate Scoliosis
Moderate scoliosis patients that we see here at the Center are given very different advice than what they would be given if they were to meet with a surgeon on the traditional treatment path.
Whether we diagnose a patient with their condition in the moderate stage, or whether they come to us with a diagnosis of moderate scoliosis, our response is always going to be proactive.
Our response is different because we want to start treatment as soon as possible.
Ideally, we catch a patient’s condition in the mild stage, and we treat it successfully so they don’t progress into the moderate stage; the same can be said of our moderate scoliosis patients. We want to treat them effectively so they don’t reach the severe scoliosis stage and have to face that decision of whether to choose surgery or not.
Our functional approach is integrative, meaning we combine multiple treatment disciplines so our patients can benefit from the merits of these different approaches and how they complement each other.
Our disciplines are scoliosis-specific and combine targeted chiropractic adjustments, exercise, therapy, and custom 3D corrective bracing.
Having an integrative approach allows us to fully customize each and every treatment plan to address the individual characteristics of the patient and their condition.
As growth occurs, we monitor to see how the spine is responding in terms of progression, and then we tweak the treatment plan by apportioning the disciplines differently as the condition necessitates.
Our treatment goal is different from the traditional approach in that we don’t want to ‘hold’ the spine in a corrective position; instead, we want to actually reduce the curvature so the condition is impacted on a structural level.
Then we want to help stabilize the correction so the spine and its surrounding muscles can support and stabilize the spine.
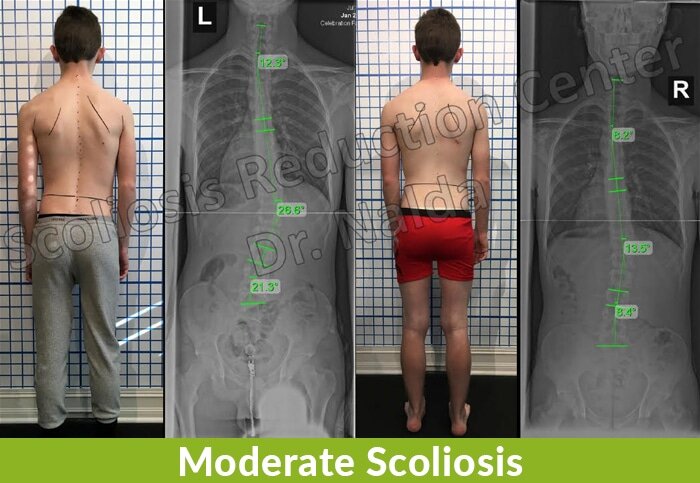
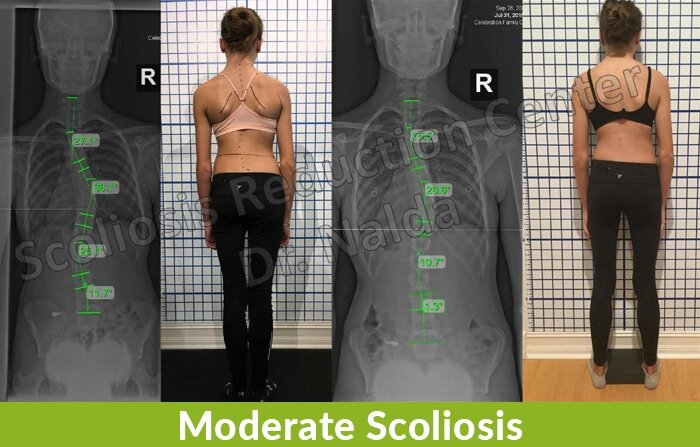
If you look at Tim’s before-and-after X-ray images, you can see the structural results of successful treatment, not to mention how the symmetry of the shoulder blades and waist line are restored.
By restoring as much of the spine’s healthy curves as possible, we are not only reducing the unhealthy ones, but also lessening related symptoms caused by the abnormal curvature.
We are also avoiding the hardships associated with moving further along the condition’s progressive line.
Bracing is often a component of treatment for moderate scoliosis in both the traditional and functional approach, but as mentioned earlier, not all braces are created equal, and this brings us to the ScoliBrace.
Bracing and Moderate Scoliosis in Functional Treatment
As we discussed the most commonly used brace in the traditional treatment approach (Boston brace), let’s explore the brace we use in our functional approach, and the differences between the two.
The modern and ultra corrective ScoliBrace represents the culmination of what the medical community has learned over the years about bracing as a potential scoliosis treatment option.
One of the differences in design between the Boston brace and the ScoliBrace is based on its differing treatment goals.
While the Boston is used to slow/stop progression, the ScoliBrace actually works towards reducing the curvature on a structural level, and then our other treatment disciplines augment those results by working towards supporting and stabilizing the reduction.
The ScoliBrace is more flexible, comfortable to wear, and thanks to our state-of-the-art scanning technology, we can fully customize the ScoliBrace to suit the patient’s body and curvature type.
The more wearer-friendly design of the ScoliBrace also helps lessen the potential issue of compliance.
The ScoliBrace not only works towards correction as its end goal, it is more customized, addresses the 3-dimensional nature of the condition, and when combined with our other active treatment disciplines, it can be a significant component of treatment success.
Now, in terms of adults with scoliosis and bracing, this is a less-common treatment option as adults, having reached skeletal maturity, are not at such a high risk of progression; while bracing used for adults with moderate scoliosis can help achieve a correction, it is more commonly used to reduce pain and stabilize the spine.
For those wanting to learn more about our alternative functional treatment approach, reach out to us here.
Scoliosis can develop at any age, which brings us to our last section: adult moderate scoliosis.
How is Adult Moderate Scoliosis Diagnosed?
When it comes to adults with moderate scoliosis, the most common forms are idiopathic and degenerative.
When moderate idiopathic scoliosis is present in adults, these cases are most commonly cases of (AIS) that remained undiagnosed until adulthood.
This is not uncommon as, previously mentioned, it’s often not until the moderate stage that people even realize they have a spinal disorder.
In these types of cases, it’s most often pain that develops as the primary symptom that becomes noticeable and brings them in to see me for an official diagnosis and treatment.
The other common form of adult moderate scoliosis is degenerative.
In adult moderate degenerative scoliosis, again, it’s most often pain that brings people in for a diagnosis.
This form is most common in adults over the age of 40 as the natural degenerative effects of aging start to impact the spine, commonly its intervertebral discs.
Once problems with the discs that separate and cushion the individual bones of the spine start to degenerate, this can cause the spine to slip out of alignment and scoliosis to develop as a result.
This form can be particularly painful as the patient is dealing with the disc problems related to spinal degeneration, plus the complication of developing scoliosis.
Conclusion
When a person develops an abnormal sideways bend to their spine that coincides with rotation and has a Cobb angle measurement of between 25 and 40 degrees, this is classified as ‘moderate scoliosis’.
Traditionally, moderate scoliosis has been somewhat of a gray area in terms of how to respond treatment-wise.
The reactive traditional approach would say, “Let’s watch and wait to see if/how fast your condition progresses,” but this means passively observing while a patient’s condition is allowed to progress.
This approach can be particularly harmful in the condition’s most common form, AIS, as this age group is entering into a stage of rapid growth and development: we know this to be the condition’s biggest trigger for progression.
In contrast, the alternative functional treatment approach we offer patients of the Scoliosis Reduction Center® is both proactive and preventative.
For our moderate scoliosis patients, our main treatment goal is two-pronged: we want to impact the condition on a structural level by reducing the abnormal curvature, and by doing this, we help patients avoid progressing into the severe stage and facing the possibility of spinal-fusion surgery.
Consultation & Information Request
If you want to schedule a consultation, or just want more information you can call 321-939-2328 or use this form. We can call or email you to discuss your options.